Medical Research Funding: Impact on Patient Safety and Ethics
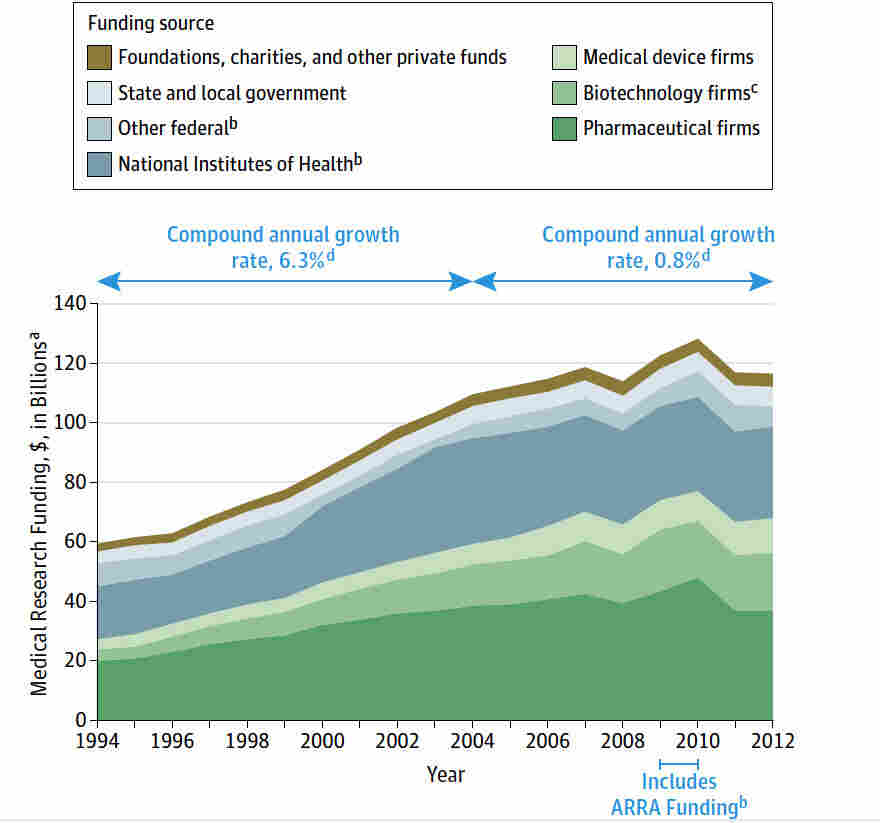
Medical research funding plays a critical role in advancing health outcomes and ensuring the safety of patients who participate in clinical studies. On the frontlines of medical innovation, it enables institutions like Harvard to develop and oversee groundbreaking research that adheres to ethical standards and regulatory compliances, safeguarding the welfare of trial participants. However, recent funding cuts have raised serious concerns about the impact on ongoing research projects and the overall patient safety in research. As institutions navigate these challenging waters, the implications of funding disruptions echo through the corridors of scientific inquiry, highlighting the fragility of progress in the face of budgetary constraints. With the National Institutes of Health (NIH) and other funders increasingly scrutinizing expenditures, maintaining robust oversight remains imperative for ethical medical research and the protection of participants.
The financial support for health-related studies, often dubbed as investment in clinical research, is fundamental to fostering advancements that improve human health. When budget limitations arise, they not only jeopardize ongoing experiments but also weaken the vital oversight mechanisms that ensure the ethical treatment of participants in these studies. The consequences of reduced funding ripple across medical institutions, affecting collaborative efforts and consequently diminishing patient safety in research endeavors. Furthermore, these financial constraints can derail the work of Institutional Review Boards (IRBs), which are essential in safeguarding medical research ethics and promoting public trust. As the landscape of medical research funding evolves, it is crucial to recognize the pivotal role these financial resources play in maintaining research integrity and public confidence.
The Importance of Medical Research Funding
Medical research funding is crucial for advancing healthcare and ensuring patient safety. This funding supports the development of new treatment protocols, innovative therapies, and medical devices that can drastically improve patient outcomes. Without adequate financial resources, research institutions may struggle to carry out vital studies that seek to understand diseases and their treatments fully. For example, the recent halt in funding has interrupted ongoing research, potentially delaying breakthroughs that could save lives or enhance the quality of health for numerous individuals.
Ample medical research funding not only enhances scientific inquiry but also strengthens the framework of patient safety protocols. It allows research teams to implement rigorous oversight mechanisms, such as Institutional Review Boards (IRBs), which play a fundamental role in protecting the rights and welfare of human participants involved in clinical trials. Disruptions in funding can lead to insufficient oversight, compromising participant safety and trust in the research process, which is essential for ethical medical practice.
Impact of Funding Cuts on Patient Safety
The recent cuts in funding pose a significant risk to patient safety within medical research. When federal grants are interrupted or eliminated, many research initiatives are forced to halt, which can lead to incomplete studies or the abandonment of critical safety assessments. The reliance on continual funding is essential for maintaining the best practices of patient safety in research, as institutions may struggle to afford the necessary reviews and oversight without financial support. This can create an environment where the ethical considerations of participant safety are compromised.
Moreover, reduced funding directly impacts the training and resources available to IRBs and research professionals tasked with ensuring ethical standards. Without adequate financial backing, these boards may not have the capability to conduct thorough reviews or address potential risks adequately. The lack of rigorous oversight can lead to situations where participants are exposed to greater risks without proper monitoring or informed consent processes being adhered to, ultimately diminishing public trust in the entire research enterprise.
The Role of Institutional Review Boards in Research Oversight
Institutional Review Boards (IRBs) play a pivotal role in safeguarding participants in medical research. They are responsible for reviewing research proposals to determine if they meet all ethical and legal standards while ensuring that the rights of participants are prioritized. IRBs not only examine informed consent processes but also assess risks, benefitting the overall integrity of the research by validating the methodologies presented. With adequate funding, IRBs can operate effectively, continuously educate researchers, and maintain compliance, thus protecting the health and safety of study participants.
In the absence of robust Institutional Review Board oversight, there can be severe consequences, including significant harm to participants and erosion of public confidence in medical research. Past historical events, like the Tuskegee Syphilis Study, serve as poignant reminders of the essentiality of ethical oversight. Funding cuts that hinder the operation of IRBs diminish their capability to uphold strict standards and protocols, putting vulnerable research populations at risk and potentially leading to repeat historical transgressions.
Ethical Implications of Research Funding Withdrawal
The ethical implications of reducing funding for medical research cannot be overstated. Individuals who volunteer for clinical trials expect that their participation will not only contribute to scientific advancement but also be respected in terms of their safety and rights. If funding cuts result in diminished oversight, it could inherently compromise research ethics, leading to scenarios where participants’ welfare is neglected to meet budgetary constraints. Ethical medical research is built on the foundation of trust, and any reduction in funding that threatens patient safety could result in a significant blow to public confidence.
Furthermore, the loss of funding can disproportionately affect studies that focus on underrepresented populations, reinforcing existing inequalities in healthcare. When funding streams become less accessible, research that addresses pressing public health issues may stall or disappear entirely, leaving vulnerable communities without adequate representation in clinical studies. This ethical consideration underscores the necessity for continued and equitable funding in medical research to ensure diverse participant safety and ethical standards.
Consequences of Stalled Clinical Trials
Stalled clinical trials due to funding cuts can have far-reaching consequences beyond the immediate research context. Participants who have committed their time and health to these studies may find themselves caught in the limbo of uncertainty, leaving them wondering about their health outcomes and the potential developments of therapies that could benefit them. This delay not only undermines their trust in the research process but also poses risks to their safety as the conditions they volunteered to be treated for may worsen in the absence of necessary interventions.
Additionally, the broader implications of halted clinical trials extend to public health and innovation on a national level. Drug and therapeutic developments heavily rely on successfully completed trials to demonstrate efficacy and safety to regulatory bodies like the FDA. When trials are halted, it stalls the entire pipeline and potentially slow the pace of scientific advancement, ultimately impacting patients who depend on new therapies to manage their conditions. The repercussions of such delays illustrate the interconnectedness of research funding and patient care.
Addressing Patient Concerns in Research
Addressing patient concerns in research is paramount for maintaining ethical standards and fostering trust. Clinical trials often present complexities that patients may find daunting. Researchers and IRBs must ensure that potential participants have clear and accessible information about the study, including potential risks and benefits. Engaging patients in dialogue about their concerns can empower them, reinforcing their autonomy in the decision-making process. Such practices improve informed consent procedures and the overall ethical framework of research.
Additionally, providing patients with avenues to express their concerns about the research and its impacts can lead to better study designs that prioritize patient safety. This incorporation of patient feedback helps ensure that research is focused on real-life implications and addresses the needs of the participants effectively. Ethical research thrives on communication and understanding; thus, fostering an environment where participants feel heard is essential for the success of clinical studies.
The Future of Medical Research Ethics
The future of medical research ethics hinges on the continuous commitment to safeguarding participant rights and well-being amid evolving scientific demands. As the landscape of medical research changes with new technologies and methodologies, ethical standards must also adapt. Ensuring that ethical considerations remain at the forefront necessitates robust funding streams, enabling institutions to train IRB members thoroughly and enforcing compliance with ethical guidelines. Future efforts must strive for a balance between innovation and the protection of human subjects.
Moreover, as funding landscapes change, it is crucial that researchers remain vigilant about the ethical implications of their work and that policy-makers recognize the need for consistent financial support. Cultivating an environment that values ethical oversight and patient safety will ultimately enhance the quality of medical research and its efficacy in developing interventions that truly address public health needs. Investing in the future of medical research ethics is paramount for ensuring that the advancements made through research are both scientifically valid and morally sound.
Restoring Trust in Medical Research
Restoring trust in medical research requires a concerted effort to recognize and address the issues arising from funding cuts. Participants must see tangible evidence of commitment to patient safety and ethical research practices. Clear communication about how funding is being utilized to support ethical oversight and participant rights can help rebuild confidence among the public. By emphasizing transparency in the research process and involving community stakeholders, institutions can begin to mend the fractures caused by funding disruptions.
Moreover, demonstrating the value of ethical practices in research through successful case outcomes can help to inspire trust and encourage greater public participation in clinical studies. Research institutions must engage with the community to better understand their concerns and perceptions of medical research. Building that bridge can enhance participation rates and ultimately lead to more robust data and improved outcomes for all stakeholders involved.
Advocating for Enhanced Research Support
Advocating for enhanced research support is critical to ensuring the continuation of high ethical standards in medical research. As funding landscapes continue to shift, researchers, institutions, and advocates must work together to highlight the importance of sustained financial support for ethical oversight initiatives. Increased awareness about the complexities of medical research and the necessity for regulations can galvanize public support for ensuring that patient safety remains paramount.
In particular, policymakers must be educated about the far-reaching consequences of funding cuts on medical research and the patient experience. Creating dialogue around the importance of NIH funding and other federal grants can help emphasize the vital role that consistent financial backing plays in maintaining ethical standards. Advocating for enhanced research support is not just about preserving the status quo – it is about pushing for advancements that prioritize patient rights and welfare in the evolving landscape of medical research.
Frequently Asked Questions
How does medical research funding impact patient safety in research studies?
Medical research funding is essential for ensuring patient safety in research studies. Funding provides resources for institutional review boards (IRBs) that oversee research protocols and protect the rights and welfare of participants. Without adequate funding, IRBs may lack the necessary support to thoroughly review studies, manage risks, and ensure compliance with ethical standards. This could lead to compromised patient safety, reduced oversight, and increased risks during research participation.
What are the consequences of funding cuts on medical research ethics?
Funding cuts can severely compromise medical research ethics. With diminished resources, institutions may struggle to uphold ethical standards in research practices, leading to inadequate oversight and increased potential for ethical violations. Research ethics rely on proper funding for training, review processes, and ethical compliance, which are crucial for protecting human subjects and maintaining public trust in clinical research.
How do NIH funding cuts affect research oversight and patient welfare?
NIH funding is vital for robust research oversight, including the operations of IRBs that safeguard patient welfare. Cuts in NIH funding can lead to resource shortages, halting ongoing studies and preventing the initiation of new trials. This undermines the integrity of research processes and can adversely affect the safety and well-being of participants, ultimately slowing biomedical advancements that benefit public health.
What role does funding play in enforcing research oversight standards?
Funding underpins the infrastructure required to enforce research oversight standards. Proper medical research funding allows for adequate staffing, training, and operational support for IRBs and oversight committees. This includes reviewing research proposals, monitoring studies for compliance, and ensuring that the ethical treatment of participants is upheld. Without sufficient funding, the enforcement of these critical oversight standards could weaken, leading to potential risks for research participants.
How can the impact of funding cuts on medical research funding be addressed?
Addressing the impact of funding cuts on medical research can involve advocacy for increased federal and state funding, fostering private-sector partnerships, and streamlining grant processes to ensure that essential studies receive financial support. Additionally, raising public awareness about the importance of medical research funding can mobilize community support and reinforce the necessity for continued investment in clinical trials, ensuring patient safety and ethical oversight in research.
What long-term effects do funding cuts have on the future of medical research?
Long-term effects of funding cuts on medical research include a slowdown in scientific progress, reduction in the number of clinical trials, and diminished patient trust in research methodologies. Funding cuts can also result in fewer qualified researchers entering the field, hinder innovation, and lead to public skepticism about the safety and efficacy of new treatments. Ensuring stable and sufficient funding is crucial for sustainable advancements in medical science.
| Key Points | Details |
|---|---|
| Impact of Funding Freeze | The Trump administration’s freeze of over $2 billion in federal research grants has disrupted patient safety and rights in medical studies. |
| Importance of IRB | Institutional Review Boards (IRBs) ensure compliance with ethical standards, protecting the welfare of research participants. |
| Role of SMART IRB | SMART IRB provides oversight across multiple research sites, improving efficiency and safety for participants. |
| Historical Context | Past medical experiments have underscored the necessity for stringent ethical oversight, such as the Tuskegee Study and WWII human trials. |
| Consequences of Cuts | Continued funding cuts could halt ongoing research, enhance public skepticism, and jeopardize the trust built within the research community. |
Summary
Medical research funding is crucial for ensuring that the safety and rights of patients enrolled in studies are effectively protected. The recent funding freeze has highlighted the importance of such financial support in maintaining ethical oversight through Institutional Review Boards (IRBs), which are essential in safeguarding human participants. Cuts in funding not only disrupt ongoing research but also undermine public trust in medical research as a whole. It is imperative that funding is restored to facilitate innovative medical advancements while ensuring participant safety.