Federal research grants play a crucial role in advancing scientific studies that address public health challenges. For researchers like Karen Emmons and Jorge Chavarro, these grants are more than mere funding; they are lifelines that enable innovative research aimed at cancer risk reduction, nutrition, and reproduction studies. The application process, particularly through the NIH grant process, is rigorous and competitive, reflecting the importance of securing research funding that can lead to meaningful health improvements. In an era where public health research faces mounting pressures and funding challenges, the value of these federal grants becomes even more significant. They represent not just financial support, but also a commitment to fostering groundbreaking research that can ultimately save lives and enhance well-being.
In the realm of scientific exploration, government-sponsored funding is pivotal for researchers dedicated to addressing critical issues like public health. These research grants from federal sources significantly impact studies related to reducing cancer risks and analyzing nutrition’s role in reproductive health. The process of obtaining such grants, especially through organizations like the NIH, involves a rigorous evaluation of proposals, ensuring that only the most impactful studies receive financial backing. For scientists, this funding is not merely about finances; it symbolizes the opportunity to innovate and make meaningful contributions to society. As public health continues to evolve, the importance of sustained support through federal research grants cannot be overstated, reinforcing the partnership between governmental bodies and academic institutions in pursuit of scientific advancement.
The Importance of Federal Research Grants in Public Health
Federal research grants are pivotal in advancing public health initiatives, enabling researchers to explore pressing health concerns and implement evidence-based solutions. These grants fund critical studies that seek to understand and mitigate health disparities across various demographics. Researchers like Karen Emmons emphasize that obtaining federal funding isn’t just a paycheck; it’s a vital resource that translates innovative ideas into tangible health improvements for communities at risk.
Moreover, the grant process fosters collaboration among scientists, policymakers, and community partners, creating a multifaceted approach to public health challenges. For example, studies funded by federal grants often address crucial areas such as cancer risk reduction and nutrition, contributing significantly to our understanding of how lifestyle changes can mitigate health risks. This interconnectedness underscores the need for sustained federal support to ensure that vital research continues to thrive and translate into real-world impact.
Navigating the NIH Grant Process: Challenges and Solutions
The NIH grant process can be daunting, marked by rigorous standards and a highly competitive atmosphere. Researchers like Jorge Chavarro outline the importance of not only crafting a compelling research proposal but also preparing extensive documentation that adheres to NIH requirements. This includes presenting evidence of prior research, supporting methodologies, and ensuring ethical considerations are meticulously followed. Researchers must demonstrate how their work innovatively fills gaps in existing knowledge, all within an application that can exceed a hundred pages.
Additionally, the selection process for NIH grants involves thorough peer evaluations, where proposals are assessed against one another based on innovation, significance, and rigor. This scrutiny ensures that only the most deserving projects receive funding, yet it can be a stumbling block for many researchers. Those whose proposals are not funded often go back to the drawing board to refine their ideas, incorporating feedback and striving for resubmission success. This iterative process serves to elevate the quality of research proposals and ultimately leads to more impactful public health outcomes.
Innovative Research in Nutrition and Reproduction Studies
Studies on nutrition and reproduction play a crucial role in understanding public health outcomes, as they explore the complex links between diet, lifestyle, and reproductive health. Jorge Chavarro’s work highlights the necessity of funding to explore these relationships further, as they can have profound implications for populations facing fertility challenges or adverse pregnancy outcomes. Through federal research grants, scientists are empowered to investigate how nutritional factors influence reproductive health, providing evidence that can inform clinical practices and public health policy.
Moreover, the findings from these nutrition and reproduction studies often extend beyond individual health to influence community health strategies. For instance, insights gained from research can help forge educational programs aimed at improving dietary habits among women of childbearing age, ultimately leading to better maternal and child health outcomes. The continued support of federal research grants is essential to drive forward these important studies, providing the framework needed to investigate and implement meaningful health interventions.
Addressing Cancer Risk Reduction Through Targeted Research
Reducing cancer risk remains one of the critical objectives of public health research from entities like the National Cancer Institute. Researchers such as Karen Emmons dedicate their efforts to understanding how specific interventions can lower cancer prevalence, particularly in underserved communities. Federal research grants are vital for these projects, funding initiatives that not only investigate risk factors but also explore community-tailored strategies effective for diverse populations.
Additionally, these studies often harness multidisciplinary approaches, integrating social sciences, biomedical research, and community engagement to develop comprehensive, effective cancer prevention programs. The significance of receiving federal funding cannot be overstated, as it alleviates the financial burden associated with conducting large-scale, impactful research that has the potential to change lives. Without such investments in research, the forward progress in cancer risk reduction and the translation of findings into actionable public health strategies would be severely limited.
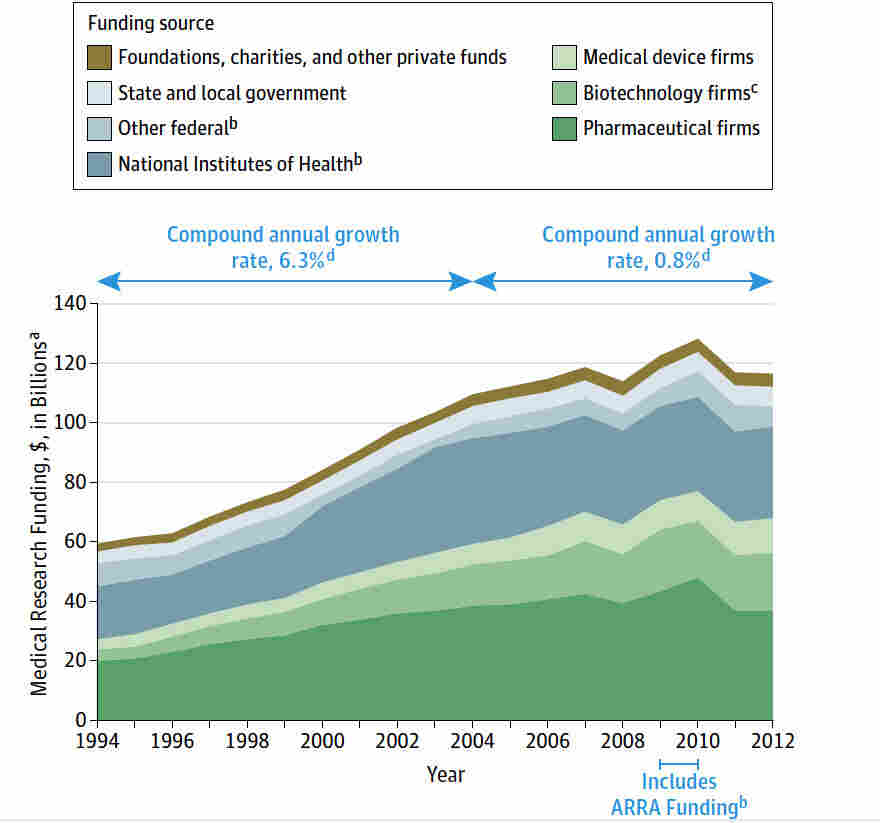
Research Funding Trends in Public Health
The landscape of research funding in public health is continually evolving, influenced by shifts in federal policy, societal needs, and emerging scientific discoveries. The fluctuating availability of federal research grants, especially in the wake of political changes, can drastically affect the research pipeline. For instance, the recent freeze on grant funding by the Trump administration posed significant challenges, stalling numerous projects and delaying advancements in critical areas of public health.
On the other hand, as communities increasingly recognize the value of preventative health measures, there has been a push for sustained investment in public health research. Funding organizations are prioritizing studies that align with current health challenges such as obesity, cancer, and mental health, ensuring that researchers have the resources necessary to tackle these pressing issues. The importance of reliable funding cannot be overstated, as it directly correlates to the capacity of researchers to innovate and implement science-driven solutions to enhance population health.
Building Partnerships for Effective Public Health Research
Collaboration is essential in public health research, as it fosters the sharing of ideas, resources, and data. Researchers like Karen Emmons emphasize the value of forming partnerships with community organizations, healthcare providers, and policy makers to enhance the relevance and applicability of their work. These partnerships can amplify research efforts, ensuring that findings are effectively translated into community-based interventions that address health disparities.
Furthermore, building strong relationships with stakeholders can also help secure additional funding opportunities, including grants from private foundations or collaborative research programs. By engaging with communities that are directly impacted by health issues, researchers are better equipped to tailor their studies to the needs of those populations, resulting in more effective and meaningful public health outcomes.
The Role of Innovation in Securing Research Grants
Innovation plays a vital role in the competitive landscape of securing federal research grants, as funding bodies are eager to support groundbreaking ideas that have the potential to revolutionize public health. Researchers must showcase not only their proposed solutions but also how their work uniquely fills existing gaps in knowledge. This innovative edge can be pivotal in distinguishing an application amidst a sea of submissions, particularly in high-stakes areas like cancer research or nutrition.
Moreover, innovative methodologies often impress reviewers, signaling a commitment to advancing science through novel approaches. Researchers who leverage technology, interdisciplinary collaboration, and community involvement can significantly enhance the perceived value of their research proposals. This focus on innovative strategies not only boosts chances of securing grants but also ultimately contributes to the advancement of public health research as a whole.
The Impact of Grant Funding on Community Health Initiatives
Federal research grants have a direct impact on community health initiatives, providing the necessary financial support to implement programs that address specific health challenges. For instance, studies focusing on nutrition and cancer prevention can lead to community outreach programs that teach people about healthy eating and lifestyle changes to reduce their risk of diseases. This kind of research-to-practice model is essential for translating findings from the lab to real-world applications.
Furthermore, grant-funded research not only supports the development of interventions but also facilitates the evaluation of their effectiveness. By establishing measurable outcomes, researchers can demonstrate the value of their initiatives, securing further funding and support from stakeholders. This cycle of funding, research, and implementation is critical for fostering healthier communities and improving public health outcomes across the board.
Best Practices for Writing Successful Grant Applications
Crafting a compelling grant application is an art form in itself, requiring attention to detail, clarity, and a comprehensive understanding of the grant’s purpose. Researchers often spend months preparing applications for federal research grants, ensuring that every aspect aligns with the funding agency’s priorities. Best practices include clear articulation of research aims, robust methodologies, and well-justified budgets, all of which strengthen an application’s competitiveness.
Additionally, seeking feedback from peers and mentors can prove invaluable in refining grant proposals. This collaborative approach not only enhances the quality of the application but can also help identify potential pitfalls before submission. Researchers should also keep abreast of changes in funding priorities and successful application trends, allowing them to adapt their strategies and approaches for future submissions.
Frequently Asked Questions
What are federal research grants and who can apply for them in public health research?
Federal research grants are funding opportunities provided by government agencies, like the National Institutes of Health (NIH), to support scientific research aimed at improving public health. Researchers, including those focusing on public health research and cancer risk reduction, can apply for these grants. Typically, any qualified principal investigator affiliated with an academic institution or research organization can submit a proposal.
How does the NIH grant process work for nutrition and reproduction studies?
The NIH grant process for nutrition and reproduction studies involves multiple stages: developing an innovative research idea, preparing a comprehensive proposal, and undergoing a rigorous review by Scientific Review Groups. Researchers must provide evidence of their methodology, significance of their study, and ethical considerations, all while justifying their budget requests. The application usually culminates in a detailed document often exceeding 100 pages.
What are the challenges researchers face when applying for federal research grants?
Researchers face significant challenges when applying for federal research grants, including strict eligibility criteria, a highly competitive environment, and the need for innovative proposals that address existing gaps in research. The limited success rates, such as the 14.6% for the R01 grant at the National Cancer Institute, highlight the difficulty in securing funding amidst a complex review process.
Why is it important for federal research grants to support public health initiatives?
Federal research grants are crucial for supporting public health initiatives because they fund studies that aim to improve community health, reduce disease impacts, and ultimately lower healthcare costs. By investing in research, such as cancer risk reduction studies, the government contributes to a healthier society and greater accessibility to essential medical advancements.
Can researchers receive feedback on unsuccessful federal grant applications?
Yes, researchers can receive feedback on unsuccessful federal grant applications. After a proposal is reviewed, applicants have the opportunity to review comments from the evaluators which can guide improvements. This process allows them to resubmit stronger proposals in future funding cycles, which is integral for continuous research development.
What role do community partnerships play in successfully obtaining federal research grants?
Community partnerships are vital for successfully obtaining federal research grants, particularly in public health and cancer risk reduction projects. Collaborating with community organizations helps researchers align their studies with real-world needs, fosters trust, and enhances the relevance and impact of their research, which can significantly strengthen grant proposals.
How do researchers justify their budgets in federal grant applications?
Researchers must provide detailed justifications for each line item in their budgets for federal grant applications. This includes explaining the necessity of every expense, such as equipment, supplies, and personnel. Clear budget justifications demonstrate the feasibility of the proposed research and its alignment with funding agency priorities.
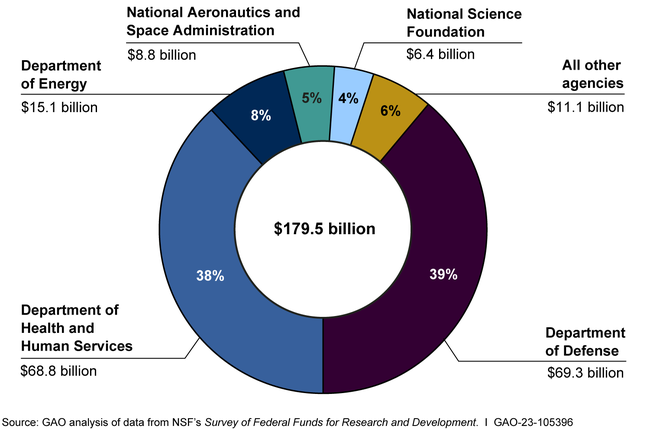
| Key Points |
Details |
| First Federal Grant Importance |
Karen Emmons recalls her first grant as a pivotal moment in her career that enabled her to help others. |
| Current Challenges |
The Trump administration froze over $2.2 billion in grants, impacting research at Harvard and halting critical studies. |
| Grant Application Process |
A six-month process involving building partnerships, testing ideas, and extensive documentation is required for submissions. |
| Evaluation and Funding Rates |
Funding success varies; at the National Cancer Institute, only 14.6% of grants received funding. |
| Public-Private Partnership |
Emmons highlights the longstanding partnership as essential for advancing science and public health. |
Summary
Federal research grants are vital for supporting groundbreaking work in public health and science, as demonstrated by the challenges faced by researchers at Harvard. Despite the hurdles in securing funding, such grants provide the means necessary for researchers like Karen Emmons and Jorge Chavarro to pursue innovative research that can lead to significant impacts on human health. The intricate process of applying for these grants not only fosters competition but also underscores the commitment to advancements that benefit society as a whole.