Age-related brain diseases, including dementia and stroke, pose significant health challenges as our population ages. Recent research has identified seventeen modifiable risk factors associated with these conditions, highlighting the potential for prevention of dementia and related disorders through lifestyle changes. Factors such as high blood pressure, poor diet, and lack of physical activity can dramatically impact brain health and overall well-being. With a focus on stroke prevention and reducing the incidence of late-life depression, these findings underscore the importance of mental health research in combating age-related illnesses. By implementing strategies to enhance brain health improvement, we can significantly reduce the toll of these diseases on individuals and society.
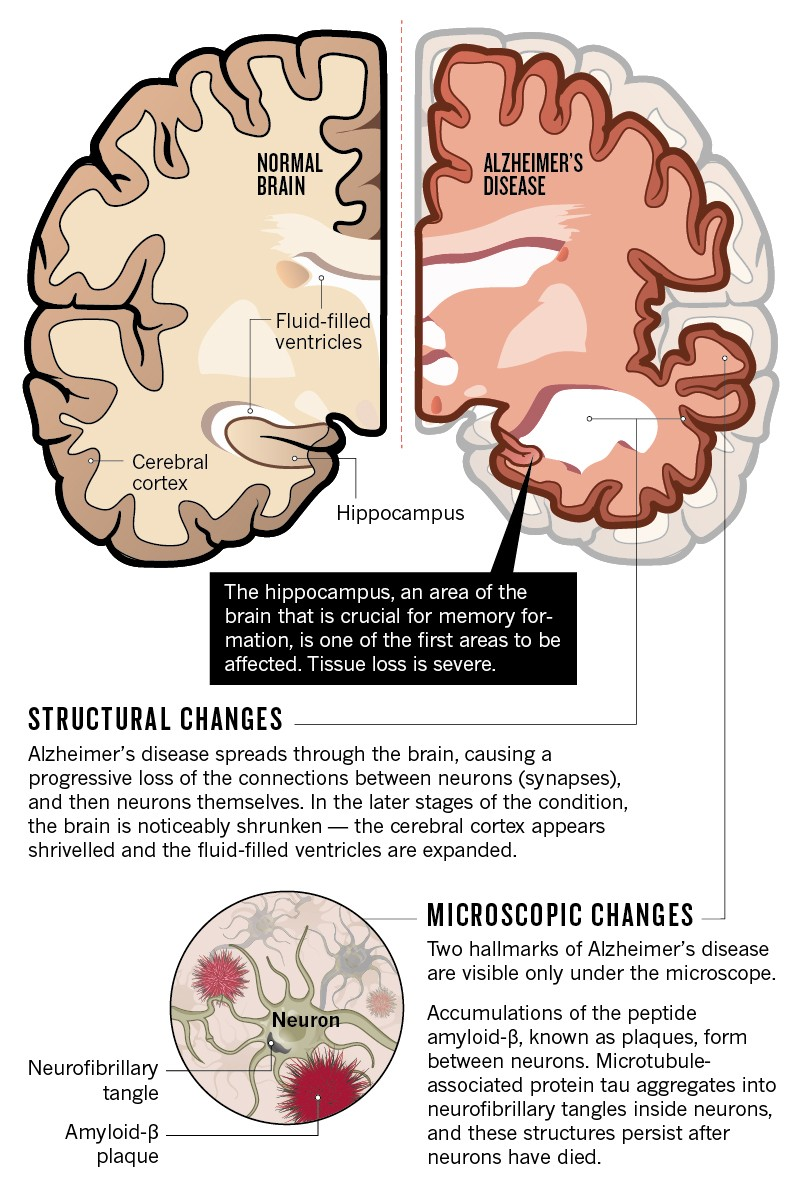
As we delve into the complexities of cognitive decline and vascular complications, age-associated neurological disorders, alternatively referred to as geriatric cognitive impairment, encompass a range of debilitating conditions that threaten quality of life. Studies are increasingly revealing interconnections among these disorders, prompting the exploration of common predictors and strategies for the prevention of dementia, especially concerning lifestyle modifications. By identifying risk factors that contribute to conditions like Alzheimer’s disease and strokes, researchers aim to arm individuals with knowledge and tools for better health management. Furthermore, concepts surrounding stroke prevention and mental wellness are gaining traction, fostering a deeper understanding of how shared lifestyle choices may lead to improved overall brain health.
Identifying Age-Related Brain Diseases Risk Factors
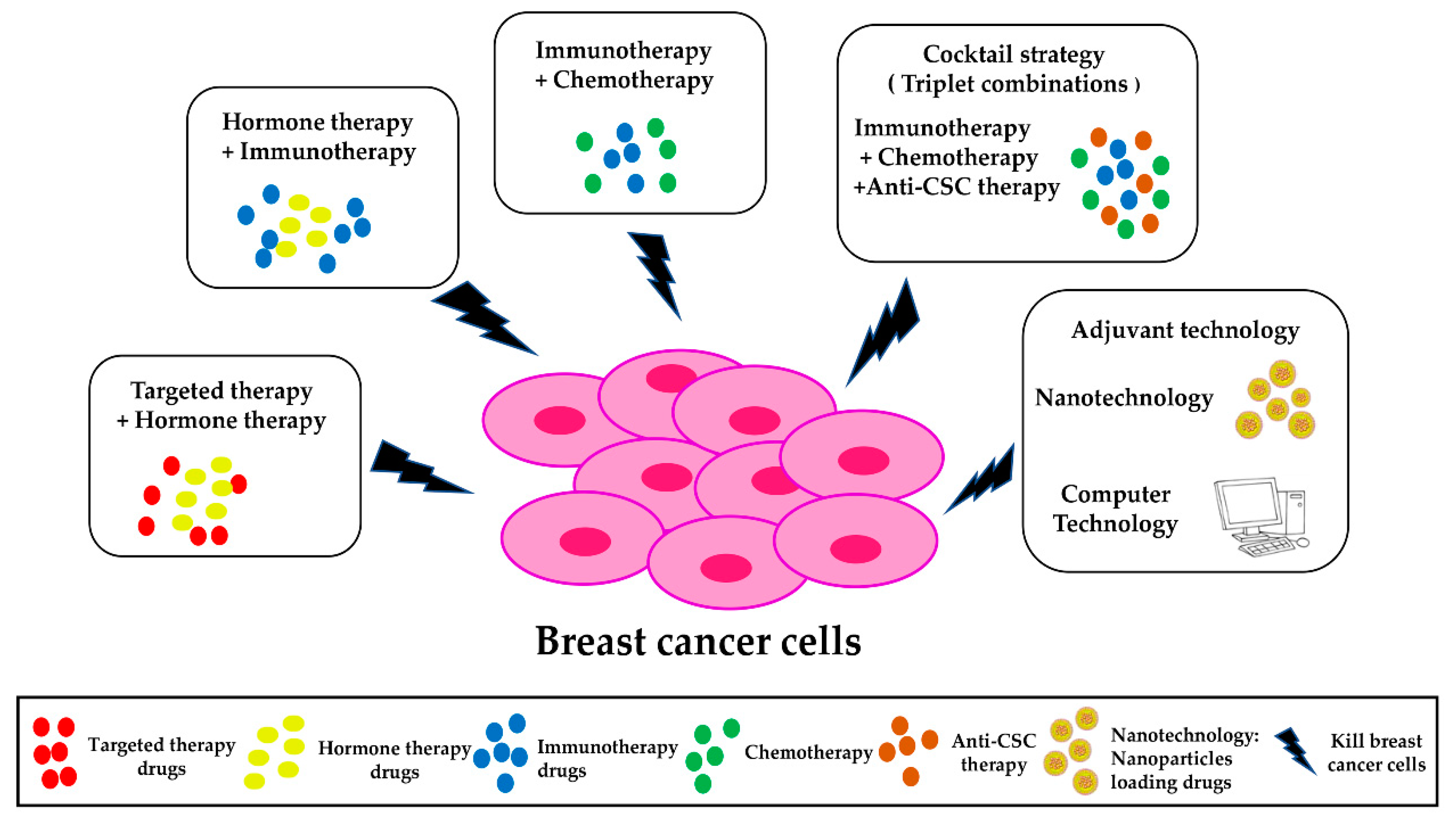
Age-related brain diseases, such as dementia and stroke, are increasingly recognized as complex conditions influenced by a multitude of risk factors. Recent research has highlighted 17 modifiable factors that significantly impact the likelihood of developing these conditions. These include not only traditional health measurements like blood pressure and cholesterol but also lifestyle choices such as diet, physical activity, and social engagement. Understanding these risk factors is crucial for individuals looking to take proactive measures toward maintaining their cognitive health.
The relationship between these factors and brain health emphasizes the importance of preventive measures. By targeting modifiable risk factors, individuals can potentially reduce their risk of stroke and dementia. For instance, engaging in regular physical activity and maintaining a balanced diet are simple yet effective strategies suggested by mental health research. Moreover, these strategies can also improve overall well-being and quality of life, highlighting that promoting brain health goes hand in hand with promoting general health.
The Role of Modifiable Risk Factors in Brain Health
Modifiable risk factors play a pivotal role in the prevention of dementia and other age-related brain diseases. Chronic conditions such as high blood pressure and diabetes have been identified as significant contributors to cognitive decline. Fortunately, these conditions can often be managed through lifestyle changes such as exercising regularly, eating a nutritious diet, and avoiding excessive alcohol consumption. Evidence suggests that individuals who adopt healthier habits can significantly reduce their risk of developing dementia or experiencing a stroke.
Additionally, mental health research underscores the impact of social engagement and purpose in life on brain health. Individuals who maintain strong social connections and find meaning in their activities tend to have better cognitive outcomes. Community programs promoting social interaction can therefore be vital in mitigating the risks associated with age-related brain diseases. Developing initiatives aimed at encouraging physical and social activities could lead to notable improvements in public health, particularly as our population ages.
Preventing Stroke: Strategies for Better Brain Health Improvisation and Lifestyle Updates Through Research: Positive Outcomes from Altered Behavior Patterns
Preventing stroke is not just a medical concern; it is also a matter of lifestyle choices that can have profound impacts on overall brain health. Researchers have found that adopting specific strategies, such as lowering blood pressure and improving diet, can effectively reduce the risk of stroke. This approach becomes even more critical when considering the intertwined nature of stroke, dementia, and depression, as they share common risk factors.
Optimizing brain health through stroke prevention can significantly lower the incidence of not only stroke but also related conditions such as dementia. Engaging in regular physical activity and maintaining a healthy weight are essential components of a comprehensive strategy. Additionally, educating the public about the importance of monitoring blood pressure and managing cholesterol can empower individuals to take control of their health and well-being.
The Connection Between Stress and Cognitive Decline
Emerging evidence suggests a strong link between chronic stress and cognitive decline, making it an essential focus in the study of age-related brain diseases. Stress activates the body’s fight-or-flight response, leading to elevated levels of cortisol, which can negatively impact brain function over time. Understanding how to manage stress effectively could play a key role in preventing dementia and stroke.
Mindfulness practices, such as meditation and yoga, have been shown to reduce stress levels and improve mental health outcomes. By cultivating resilience against stressful situations, individuals can enhance their overall brain health. Incorporating stress management techniques into daily life can serve as a protective factor against the development of age-related cognitive disorders, further emphasizing the need for ongoing research and community education in mental health strategies.
The Importance of Physical Activity for Brain Health
Physical activity is consistently highlighted as a pivotal modifiable factor for enhancing brain health and preventing age-related diseases. Regular exercise boosts blood flow to the brain, promoting neurogenesis and reducing the risk of cognitive decline. Studies show that individuals who engage in moderate physical activity experience a lower incidence of both stroke and dementia, further linking lifestyle choices to mental acuity.
Moreover, incorporating physical activity into daily routines can also have beneficial effects on mental health, reducing symptoms of depression and anxiety. As researchers continue to explore the benefits of an active lifestyle, it becomes increasingly clear that promoting physical activity is an effective strategy for improving cognitive health across the lifespan. Communities should prioritize initiatives that encourage regular exercise, especially among older adults, to foster better mental and physical well-being.
Nutritional Impact on Cognitive Health
Nutrition plays a crucial role in maintaining cognitive health, with various studies indicating a direct correlation between diet and the risk of age-related brain diseases. Diets rich in fruits, vegetables, whole grains, and healthy fats are associated with lower risks of dementia and stroke. For example, the Mediterranean diet, known for its emphasis on healthy fats and antioxidants, has been found to support brain health by reducing inflammation and oxidative stress.
Conversely, poor dietary choices, such as high sugar intake and processed foods, can contribute to increased risk factors like obesity and high cholesterol, which are linked to cognitive decline. Therefore, advocating for nutritional education and access to healthier food options in communities can significantly impact public health, potentially diminishing the burden of age-related cognitive disorders while supporting overall health.
Understanding the Role of Social Engagement in Mental Health
Social engagement is a vital component in the context of mental health and age-related brain diseases. Frequent interaction with family and friends not only enhances quality of life but also serves as a protective factor against cognitive decline. Studies find that individuals who maintain strong social ties are less likely to experience depression and the accompanying risks of stroke and dementia, showcasing the importance of community connections.
Encouraging participation in social activities and fostering environments that promote social interactions can significantly contribute to mental health improvement. This aspect should be incorporated into preventive strategies targeting age-related brain diseases. By addressing the social dimensions of well-being, health professionals can cultivate more comprehensive programs dedicated to enhancing longevity and brain health.
Exploring the Impact of Sleep Quality on Cognitive Function
Sleep quality is often underestimated in its role in supporting cognitive function and overall brain health. Research indicates that poor sleep patterns can elevate the risks of developing age-related diseases such as dementia and stroke. During sleep, the brain undergoes processes that aid in memory consolidation and detoxification, underscoring the necessity for consistent, restful sleep to maintain cognitive clarity.
Many individuals struggle with sleep due to stress, lifestyle, and aging, yet making sleep a priority is essential for brain health. Establishing healthy sleep habits—such as creating a bedtime routine, minimizing screen time, and managing stress—can have lasting benefits. Prioritizing sleep hygiene is an effective and often overlooked strategy in the fight against cognitive decline, proving beneficial for both mental health and the prevention of age-related brain diseases.
The Need for Continued Research on Modifiable Risk Factors
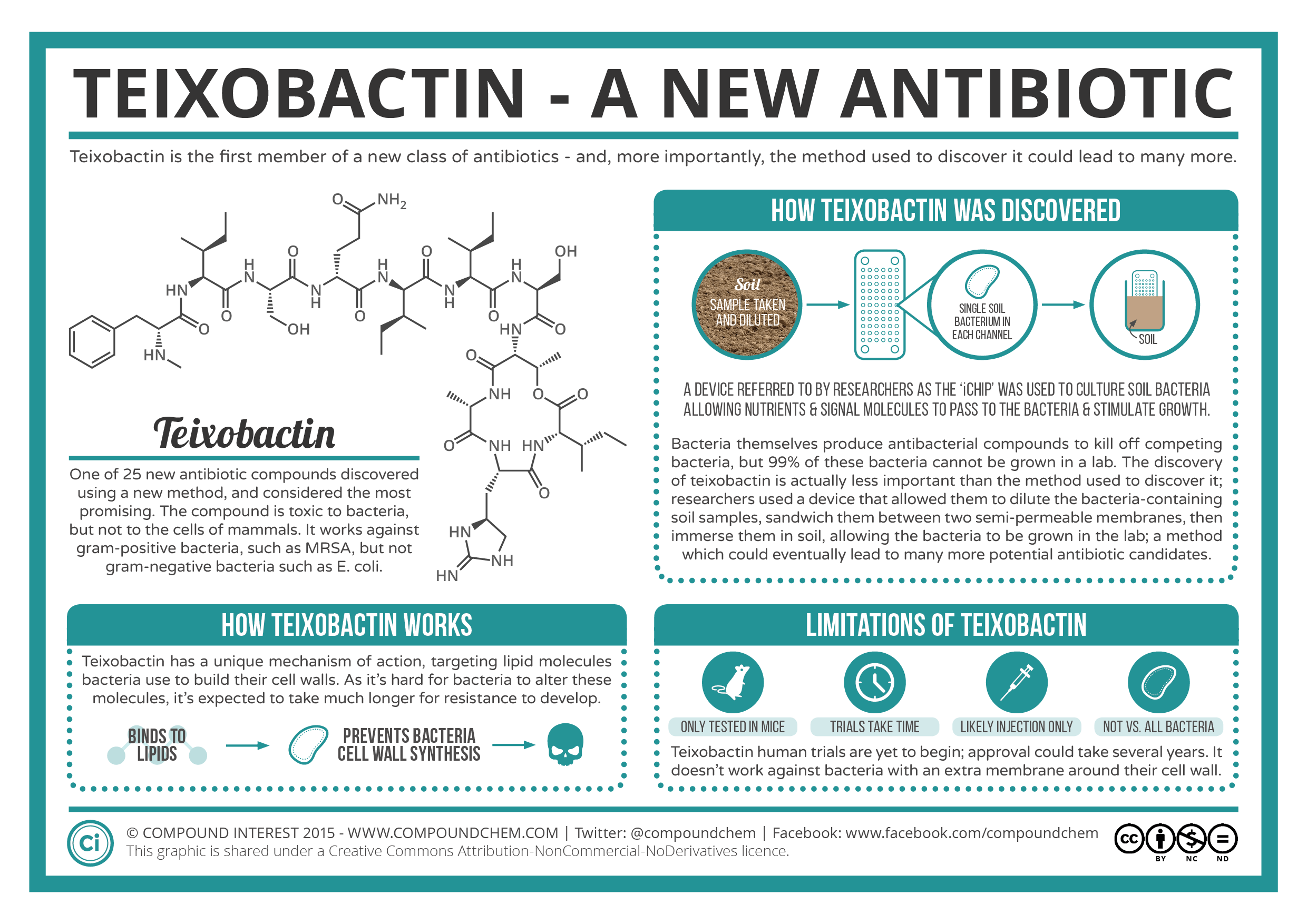
The identification of modifiable risk factors has opened new avenues for research and intervention in the realm of age-related brain diseases. Continued exploration into how behavioral changes can influence dementia, depression, and stroke risk is crucial for developing effective preventive strategies. This research can lead to innovative programs and tools, such as the Brain Care Score, designed to help individuals understand their risk and take actionable steps.
As our understanding of the interplay between health behaviors and brain health deepens, it becomes increasingly vital to emphasize the importance of education and awareness. Encouraging individuals to adopt healthier lifestyles and manage their risks can have profound effects, not only on personal health outcomes but also on public health initiatives designed to lower the prevalence of age-related cognitive disorders.
Frequently Asked Questions
What are modifiable risk factors for age-related brain diseases?
Modifiable risk factors for age-related brain diseases, such as dementia and stroke, are lifestyle and health-related aspects that individuals can change to reduce their risk. These include managing blood pressure, controlling blood sugar, maintaining a healthy diet, engaging in regular physical activity, reducing alcohol consumption, quitting smoking, and fostering social connections. By addressing these factors, individuals may lower their chances of developing age-related brain diseases.
How can I prevent dementia through lifestyle changes?
Preventing dementia involves implementing critical lifestyle changes aimed at reducing modifiable risk factors. Key strategies include maintaining a balanced diet, engaging in regular physical exercise, staying socially active, managing stress, ensuring quality sleep, and controlling chronic conditions like diabetes and hypertension. Research indicates that these actions can significantly lower the risk of developing dementia and improve overall brain health.
Is there a link between stroke prevention and age-related brain diseases?
Yes, there is a strong link between stroke prevention and age-related brain diseases. Many of the same modifiable risk factors, such as high blood pressure, diabetes, and obesity, increase the risk of both strokes and conditions like dementia. Effective management of these risk factors can not only prevent strokes but also mitigate the risk of developing dementia and late-life depression, highlighting the importance of a comprehensive approach to brain health.
What role does mental health research play in understanding age-related brain diseases?
Mental health research plays a crucial role in understanding age-related brain diseases by identifying the connections between mental health conditions, such as depression, and neurological diseases like dementia and stroke. Research has shown that untreated mental health issues can exacerbate the risk of these brain diseases. By exploring these relationships, researchers can develop effective prevention strategies and interventions, which may lead to improved brain health and quality of life for older adults.
How can physical activity improve brain health in older adults?
Physical activity has a significant positive impact on brain health, especially in older adults. Engaging in regular exercise helps improve blood flow to the brain, reduces the risk of diseases like hypertension and diabetes, and enhances cognitive function. By incorporating physical activity into daily routines, older adults can lower their risk of developing dementia, stroke, and late-life depression, thereby promoting overall brain health and wellbeing.
What is the Brain Care Score and its significance in preventing age-related brain diseases?
The Brain Care Score is a tool developed by researchers to provide a comprehensive assessment of an individual’s brain health based on modifiable risk factors. This score helps individuals understand their current risk of age-related brain diseases and offers guidance on lifestyle changes that can enhance brain health. By utilizing the Brain Care Score, individuals can take proactive steps to reduce the risk of conditions like dementia, stroke, and depression, aligning with recent findings in mental health and neurological research.
How does social engagement affect the risk of age-related brain diseases?
Social engagement has been shown to significantly lower the risk of developing age-related brain diseases, including dementia and depression. Staying socially active fosters mental stimulation and emotional support, both of which are essential for brain health. Lack of social interaction can increase feelings of loneliness and depression, which are risk factors for cognitive decline, making it important for older adults to maintain social connections to protect against age-related brain diseases.
What dietary changes can reduce the risk of age-related brain diseases?
To reduce the risk of age-related brain diseases, individuals should focus on a nutrient-rich diet. This includes consuming plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats while avoiding excessive sugar, saturated fats, and processed foods. A balanced diet supports brain health by managing factors like obesity, diabetes, and cholesterol levels, which are all linked to an increased risk of dementia and stroke. Following dietary guidelines can significantly enhance cognitive resilience in aging populations.
| Risk Factor | Impact on Age-Related Brain Diseases |
|---|---|
| Diabetes | Increases risk for stroke, dementia, and depression |
| Blood Pressure | Major risk factor for all three conditions |
| Kidney Disease | Increases risk of stroke, dementia, and depression |
| Fasting Plasma Glucose | High levels increase risk for all three conditions |
| Total Cholesterol | High levels increase risk of stroke and dementia |
| Alcohol Use | Excessive consumption linked to all three conditions |
| Diet | Poor diet can contribute to all conditions |
| Hearing Loss | Modifiable risk factor for dementia |
| Pain | Chronic pain increases risk of depression |
| Physical Activity | Lack of activity is a risk factor for all three conditions |
| Purpose in Life | Lack of purpose contributes to depression |
| Sleep | Poor sleep quality increases risk of depression |
| Smoking | Major risk factor for stroke, dementia, and depression |
| Social Engagement | Lack of engagement contributes to depression |
| Stress | Chronic stress increases risk of depression |
| Obesity | Risk factor for stroke, dementia, and depression |
Summary
Age-related brain diseases pose significant public health challenges, with conditions like stroke, dementia, and late-life depression showing interconnected risk factors. By understanding and modifying these factors—such as high blood pressure, diabetes, and smoking—individuals can potentially reduce their risk of these debilitating conditions. The recent findings emphasize that preventative measures can be straightforward, highlighting the importance of lifestyle changes to improve overall brain health and well-being.